FHIR API: HL7 DaVinci
GenHealth is able to seamlessly integrate with any FHIR server implementing the HL7 DaVinci specification for prior authorization
Integration with HL7 DaVinci FHIR APIs
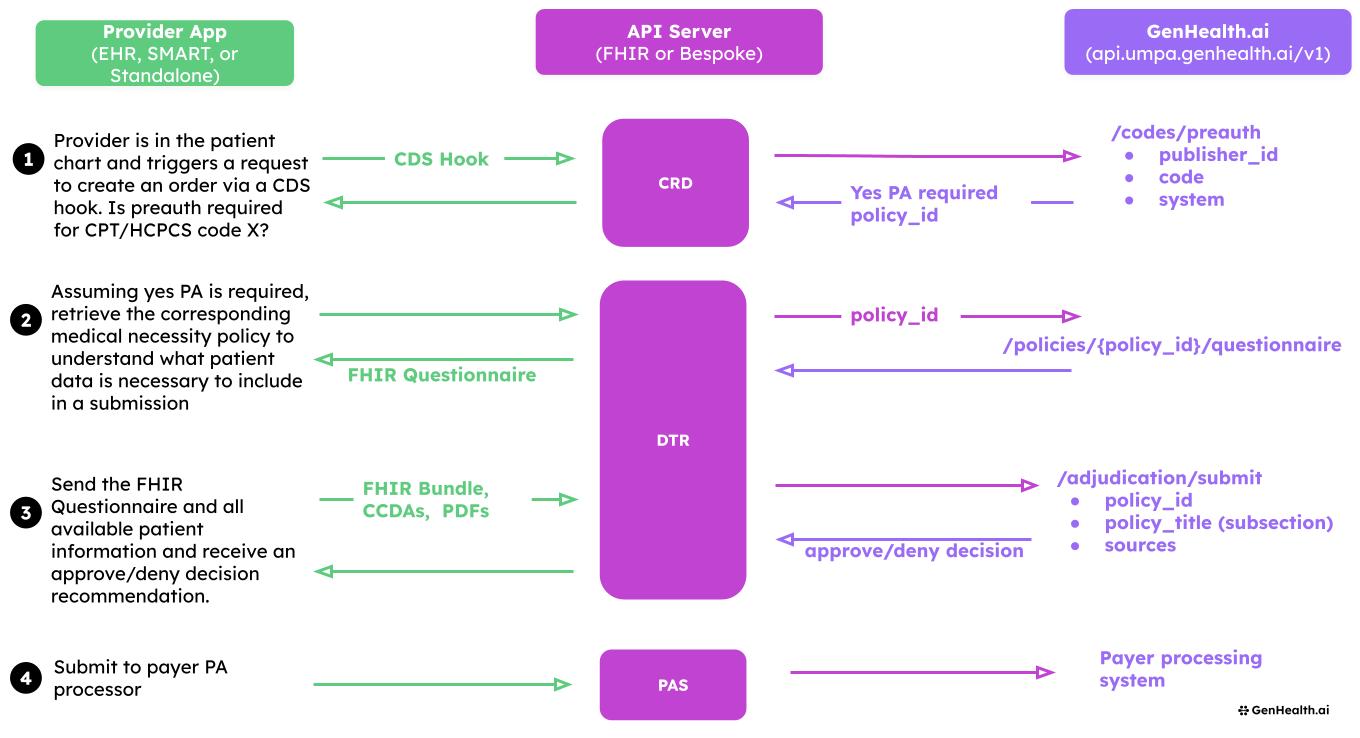
The UMPA API fully integrates with the HL7 Da Vinci project's FHIR-based implementation guides, supporting seamless interoperability in the healthcare ecosystem. This integration covers three key areas of the prior authorization process:
- Coverage Requirements Discovery (CRD)
- Documentation Templates and Rules (DTR)
- Prior Authorization Support (PAS)
GenHealth API as Payer Interface
The GenHealth API functions as a payer interface, surfacing information that needs to be returned to the FHIR API in a simple, standardized format. This functionality streamlines the communication between providers and payers, making it easier to retrieve and interpret coverage requirements, documentation needs, and authorization decisions.
Coverage Requirements Discovery (CRD)
The CRD integration allows healthcare providers to automatically discover coverage requirements, including prior authorization and documentation needs, at the point of service.
Key features:
- Real-time querying of payer systems for coverage requirements
- Automatic identification of services requiring prior authorization
- Seamless integration with EHR systems for workflow efficiency
- GenHealth API acts as an intermediary, simplifying payer responses for easy consumption
- Surfaces CPT, HCPCS, or ICD codes that require prior authorization through our /preauth/codes endpoint
Documentation Templates and Rules (DTR) and Prior Authorization Support (PAS)
DTR integration provides dynamic, context-sensitive questionnaires to gather required information for prior authorization requests.
Key features:
- FHIR-based questionnaires tailored to specific procedures and payer requirements
- Pre-population of questionnaires with available patient data
- Support for complex logic and decision trees in documentation requirements
- GenHealth API translates payer-specific requirements into standardized FHIR questionnaires
- Generates a decision tree from any medical policy document and surfaces the output as a questionnaire
- Can convert from PDF policy to FHIR questionnaire in seconds
- Option to return output as Clinical Quality Language (CQL)
Prior Authorization Support (PAS)
PAS integration enables the electronic submission and real-time adjudication of prior authorization requests.
Key features:
- Structured submission of prior authorization requests using FHIR resources
- Real-time status updates on submitted requests
- Support for attachments and additional documentation
- GenHealth API facilitates communication between provider systems and payer adjudication engines
- Can fill out a patient chart against medical policy and return a decision
- Supports both automated decisions and routing through human review in a Utilization Management department
Getting Started with Da Vinci Integration
For more information on how to implement these integrations in your FHIR server, please reach out [email protected]
Updated 12 months ago